
Apr 15, 2024 / Traumatic Brain Injury
Sexuality following Acquired Brain Injury
Sexuality is a natural part of life and an integral part of our human experiences. This includes physically, spiritually, psychologically. Sexual dysfunction is common amongst acquired brain injury survivors. 57-75% of survivors suffer from some form of sexual dysfunction to include decreased or increased sexual desire, decreased arousal, difficulty or inability to reach orgasmic climax and reproductive changes.
“Acquired physical and mental impairments may significantly alter, yet do not eliminate basic sexual drives or human needs for affection, intimacy, and a healthy positive self-concept” (Medlar, 1998)
There are many myths associated with sexuality following an acquired brain injury:
There are challenges present in the rehabilitation setting due to lack of awareness and training for rehabilitation professionals as well. Unfortunately, brain injury survivors and their families receive minimal information about the potential changes in sexual functioning following injury. Rehabilitation professionals may feel challenged by this topic, may avoid or overreact to conversations with clients and feel as though it may not be their role to discuss. With insufficient training and support and education offered to staff, patient behaviors tend to be viewed in a negative way with staff describing them as pathological and erratic, contributing it to impulsivity.
Approaches the rehab professional could take include the following:
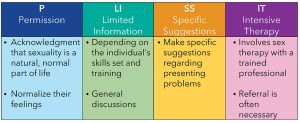
The PLISSIT Model can also be a useful guide for rehab professionals to understand their role in this process:
“A key part of human life is the ability to create and sustain intimate relationships” (Shah, 2009)
There are ways to approach sexual intimacy with our clients. Understanding that intimacy can occur with and without sex is important. This could include warmth and closeness with and without touch, verbal expressions of love, and quality time. Counseling is recommended for individuals and couples when appropriate. Areas of focus could be:
There are also ways to assist individuals connect with others which could include social media, support groups, ABI camps and community events, and video chats with others.
Sexuality contributes to our quality of life, sense of worth, desirability and self-esteem and is a natural part of our experience as humans. Let’s talk about sex with our patients, their families and our rehabilitation teams.
Resources:
Better Health Channel – https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/brain-injury-and-sexual-issues
Brain Injury Association of America – https://www.biausa.org/public-affairs/media/sex-gender-and-traumatic-brain-injury-implications-for-better-science-and-practice
Model Systems Knowledge Translation Center – https://msktc.org/tbi/factsheets/sexuality-after-traumatic-brain-injury
Paige Salinas is the vice president of clinical operations for Learning Services, A Collage Rehabilitation Partner. She leads interdisciplinary teams in their Colorado, Utah and California programs.